Andrew Weil, a major proponent of the idea of self-healing (
1), has repeatedly acknowledged the influence of osteopaths such as Robert C. Fulford (
2) on him, particularly regarding his philosophy of health management. Self-healing is not about completely autonomous healing; it is about healing by stimulation of the body's self-repair processes, which in some cases can be achieved by simply reducing stress.
Interestingly, there are many reported cases of osteopaths curing people from various diseases by doing things like cranial manipulation and other forms of touching. We also have much evidence of health improvement through prescription of drugs that don’t appear to have any health benefits, which is arguably a similar phenomenon.
The number of such reported cases highlights what seems to be a reality about diseases in general, which is that they often have a psychosomatic basis. Their “cure” involves making the person affected believe that someone can cure him, a healer, with or without drugs. The healer then cures the person essentially by her power of suggestion.
Paleoanthropological evidence suggests that this healer-induced phenomenon has always been widespread among hunter-gatherer cultures, so much so that it may well have been the result of evolutionary pressures. If this is correct, how does it relate to health in our modern world?
I am very interested in hunter-gatherer cultures, and I have also been living in Texas for almost 10 years now. So it is only natural for me to try to learn more about the former hunter-gatherer groups in Texas, particularly those who lived in the area prior to the introduction of horses by the Europeans.
There are parks, museums, and other resources on the topic in various parts of Texas, which are at driving distance. Unfortunately much has been lost, as the Plains Indians of Texas (e.g., Comanches and Kiowas) who succeeded those pre-horse native groups have largely been forcibly relocated to reservations in Oklahoma.
Anthropological evidence suggests that the earliest migrations to America have occurred via the Bering Strait, initially from Siberia into Alaska, and then gradually spreading southward to most of the Americas between 13,000 and 10,000 years ago.
Much of what is known about the early Texas Indians is due to Álvar Núñez Cabeza de Vaca, a Spanish explorer who survived a shipwreck and lived among the Amerindians in and around Texas between 1528 and 1536. He later wrote a widely cited report about his experiences (
3).
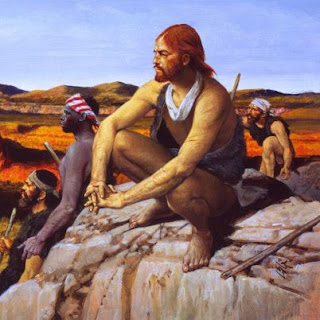
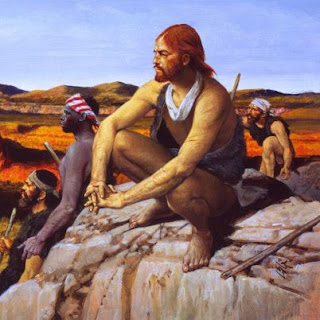 (Cabeza de Vaca and his companions; source: Biography.com)
(Cabeza de Vaca and his companions; source: Biography.com)
In Spanish, “cabeza de vaca” means, literally, “cow’s head”. This odd surname, Cabeza de Vaca, clearly had a flavor of nobility to it in Spain at the time.
You may have heard that early American Indians were uniformly of short stature, not unlike most people at the time, but certainly shorter than the average American today. Cabeza de Vaca dispels this idea with his description of the now extinct Karankawas, a description that has been born out by anthropological evidence. The male members “towered above the Spaniards”, often 6 ft or taller in height, in addition to being muscular.
The Karankawas were a distinct indigenous group that shared the same environment and similar food sources with other early groups of much lower stature. This strongly suggests a genetic basis for their high stature and muscular built, probably due to the “founder effect”, well known among population geneticists.
Cabeza de Vaca and three companions, two Spaniards and one Moroccan slave, were believed by the Amerindians to be powerful healers. This enabled them to survive among early Texas Indians for several years. Cabeza de Vaca and his colleagues at times acknowledged that they were probably curing people through what we would refer today as a powerful placebo effect.
Having said that, Cabeza de Vaca has also come to believe, at least to a certain extent, that he was indeed able to perform miraculous cures. He repeatedly stated his conviction that those cures were primarily through divine intervention, as he was a devout Christian, although there are many contradictory statements in this respect in his reports (possibly due to fear from the Spanish Inquisition). He also performed simple surgeries.
Much has been written about Cabeza de Vaca’s life among the early Indians of Texas and surrounding areas, including the report by Cabeza de Vaca himself. One of my favorites is the superb book “A Land So Strange” (
4) by Andrés Reséndez, a professor of history at the University of California at Davis (
5).
The Spanish explorer’s experiences have been portrayed in the film “Cabeza de Vaca” (
6), which focuses primarily on the supernatural angle, with a lot of artistic license. I must admit that I was a bit disappointed with this film, as I expected it to show more about the early Indians’ culture and lifestyle. Juan Diego, the Spanish actor portraying Cabeza de Vaca, was razor thin in this film - a fairly realistic aspect of the portrayal.
It is quite possible that modern humans have an innate tendency to believe in and rely on the supernatural, a tendency that is the product of evolution. We know from early and more recent evidence from hunter-gatherer societies that supernatural beliefs help maintain group cohesion and, perhaps quite importantly, mitigate the impact that the knowledge of certain death has on the mental health of hunter-gatherers.
Homo sapiens is unique among animals in its awareness of its own mortality, which may be a byproduct of its also unique ability to make causal inferences. Supernatural beliefs among hunter-gatherers almost universally address this issue, by framing death as a threshold between this existence and the afterlife, essentially implying immortality.
Yet, supernatural beliefs seem to also have a history of exploitation, where they are used to manipulate others. Cabeza de Vaca himself implies that, at points, he and his companions took personal advantage of the beliefs in their healing powers by the various indigenous groups with which they came into contact.
Modern humans who are convinced that they have no supernatural beliefs often perceive that to be a major advantage. But there could be disadvantages. One is that they may have more difficulty dealing with psychosomatic disorders. The conscious knowledge that they are psychosomatic could possibly pale in comparison with the belief in supernatural healing, in terms of curative power. Another potential disadvantage is a greater likelihood of suffering from mental disorders.
Finally, those who are sure that they have no supernatural beliefs; are they really correct? Well, subconsciously things may be different. Perhaps a good test would be to go to a “convincing” movie (i.e., not a laughable “B-level” one; for lack of a better word) about supernatural things, such as possession or infestation by evil spirits, and see if it has any effect on you.
If the experience does have an effect on you, even a small one, couldn't this suggest that your subconscious belief in the supernatural may not be so easy to control in a conscious way? I suspect that having no supernatural beliefs is unnatural and unhealthy. In most cases it probably creates a conscious-subconscious conflict, and a fairly pessimist view of the world.
My guess is that it is better to have those beliefs, in some form or another, and be on guard against exploitation.
His degrees are in electronics engineering (B.E.E.), computer science (M.S.), and business management (Ph.D.). Two of his main areas of formal academic research are nonlinear variance-based structural equation modeling, and evolutionary biology as it applies to the study of human-technology interaction. He also conducts independent research on health-related issues. Selected publications and contact informaton are available from his academic page, on the link above.
He started developing software while in high school, and has developed software tools to automate various processes, including business analytics and data mining, detection and correction of deformities in metal axles, error detection and correction in telecommunication devices, health data analysis, inventory control, invoice management, optical character recognition, stock price analysis, structural equation modeling, and travel management.
His views expressed in blogs and elsewhere are his own and do not represent the views of his employer or any organization funding his research. He is not a medical doctor, and thus readers of his Health Correlator blog and other health-related writings should consult with their own medical doctors about their health.